At askdoctor.ai, we’re committed to providing clear, trustworthy information to help you better understand and manage conditions that affect your daily comfort, like seasonal allergies and non-allergic rhinitis. Whether you’re dealing with constant congestion, sneezing, or unexplained nasal symptoms, knowing the difference between these two conditions is the first step toward lasting relief.
This article breaks down the key differences between seasonal allergies and non-allergic rhinitis in plain, easy-to-understand language. You’ll learn about common symptoms, what causes each condition, how they’re diagnosed, and which treatments are most effective. We’ll also share practical tips, expert-backed strategies, and inspiring success stories to help you breathe easier and regain control of your health.
Whether you’re seeking answers for yourself or supporting someone you care about, our goal is to provide helpful, empowering guidance—so you can feel better, live better, and enjoy every season without worry.
Allergies or Rhinitis: The Battle Behind Your Constant Congestion
If you’re constantly sneezing, sniffling, or feeling stuffed up, you’re not alone. But is it just seasonal allergies, or could it be something else? Many people confuse allergic reactions with a lesser-known culprit: chronic (non-allergic) rhinitis. Understanding the difference is key to finding real, lasting relief.
In this article, we’ll unpack the causes, symptoms, and treatments for both conditions—so you can finally get to the bottom of your congestion and breathe easier every day.
Allergies vs. Rhinitis: How They Work and How to Tell the Difference
If you struggle with a stuffy nose, sneezing fits, or constant congestion, you may be dealing with either allergies or rhinitis—but knowing which one is key to getting the right treatment.
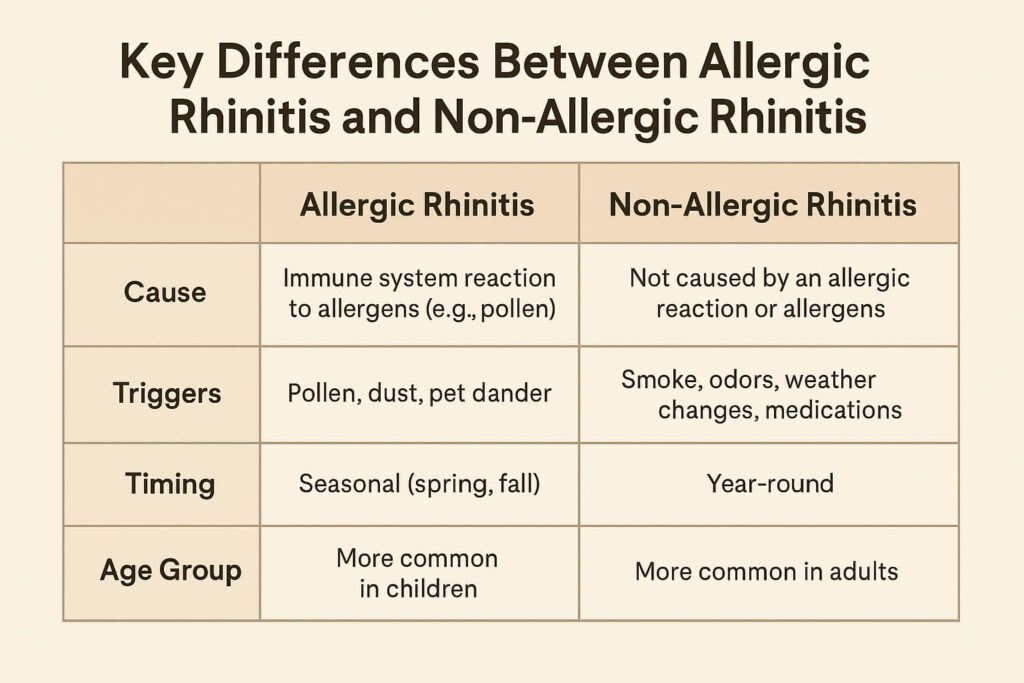
Allergies occur when your immune system overreacts to harmless substances like pollen, dust mites, or pet dander. This immune response triggers symptoms such as sneezing, itchy eyes, and nasal congestion, especially during certain seasons.
Rhinitis, on the other hand, refers to inflammation of the nasal lining. It can be allergic (triggered by allergens) or non-allergic (caused by things like changes in weather, strong odors, or infections). Unlike allergic rhinitis, non-allergic rhinitis isn’t driven by the immune system, which makes it harder to pinpoint and manage.
What Are Seasonal Allergies?
Seasonal allergies—also known as hay fever or allergic rhinitis—happen when your immune system overreacts to allergens like pollen or mold, which are more common during certain times of the year.
Common Triggers
- Tree pollen (spring)
- Grass pollen (late spring to summer)
- Weed pollen (late summer to fall)
- Mold spores (especially in humid or damp environments)
These allergens enter your nose or eyes and trigger symptoms like sneezing, congestion, runny nose, and itchy eyes—classic symptoms of hay fever.
Who Is Most Affected?
- Children and young adults often show the first signs.
- People living in areas with high pollen counts (e.g., rural or suburban environments) are more prone.
- A family history of allergies increases risk.
Seasonal Timing
- Spring: Tree pollen
- Summer: Grass pollen
- Fall: Weed pollen and mold
- Winter: Rare, but indoor allergens like dust mites and mold can still trigger symptoms
What Is Non-Allergic Rhinitis?
Non-allergic rhinitis is a condition that causes chronic sneezing, nasal congestion, or a runny nose, just like allergies, but without an allergic reaction or immune system trigger. That means it’s not caused by pollen, dust, or pet dander.
How It Differs from Allergies
Unlike allergic rhinitis (like hay fever), non-allergic rhinitis does not involve the immune system or allergic antibodies. Allergy tests come back negative. The symptoms are real, but the cause is usually irritation or inflammation, not allergens.
Common Triggers
- Strong odors (perfume, cleaning products)
- Smoke or pollution
- Weather changes (cold air, humidity)
- Spicy foods
- Alcohol
- Hormonal changes (e.g., pregnancy)
- Medications (e.g., nasal decongestant overuse)
Who Is More Likely to Experience It?
- Adults over 20 (more common than in children)
- People exposed to irritants or with sensitivities to environmental factors
- Often seen in people with asthma or eczema, though not always related
Seasonal Timing (Non-Allergic Rhinitis)
- Spring: Temperature shifts, strong floral scents, increased air irritants
- Summer: Heat, humidity, air conditioning, scented products
- Fall: Cool air, fireplace smoke, mold from leaves
- Winter: Dry indoor air, cold outdoor air, strong indoor odors
Symptoms: What to Watch For
Shared Symptoms of Allergic and Non-Allergic Rhinitis
Both allergic and non-allergic rhinitis can produce similar discomforts that affect your nose and sinuses. Common symptoms include:
- Nasal congestion
- Runny nose (rhinorrhea)
- Sneezing
- Postnasal drip (mucus dripping down the throat)
- Decreased sense of smell
- Sinus pressure or facial pain
These overlapping symptoms can make it difficult to tell the two conditions apart without a proper diagnosis.
Unique Signs of Allergic Rhinitis
Allergic rhinitis is triggered by allergens like pollen, dust mites, mold, or pet dander. Its symptoms often include:
- Itchy nose, throat, or eyes
- Red, watery, or puffy eyes (allergic conjunctivitis)
- Symptoms that occur seasonally or after exposure to specific allergens
- Worsening symptoms outdoors (e.g., during pollen season)
These symptoms usually begin shortly after exposure to allergens and may follow a pattern, especially with seasonal allergies.
Unique Signs of Non-Allergic Rhinitis
Non-allergic rhinitis isn’t triggered by allergens but by irritants or internal factors such as:
- Strong odors (perfume, cleaning products)
- Changes in temperature or humidity
- Spicy foods or alcohol (gustatory rhinitis)
- Symptoms that occur year-round without a seasonal pattern
- No itching in the eyes or throat
Unlike allergic rhinitis, non-allergic rhinitis doesn’t involve the immune system and is less likely to be accompanied by eye symptoms or itching.
When to See a Doctor
Whether symptoms are due to allergic or non-allergic rhinitis, you should seek medical advice if:
- Symptoms persist for more than 10 days
- Over-the-counter medications provide little or no relief
- You experience frequent sinus infections
- Breathing through your nose becomes consistently difficult
- Symptoms interfere with sleep, school, work, or quality of life
- You’re unsure of the cause (to rule out allergies or structural issues)
An ENT specialist or allergist can help identify the exact cause and recommend effective treatments like allergy testing, nasal sprays, or lifestyle changes.
Diagnosis: How to Know Which One You Have
Medical History and Symptom Tracking
The first step in diagnosing allergic vs. non-allergic rhinitis is a detailed review of your medical history and symptoms. Your doctor will likely ask about:
- When symptoms occur (seasonal, year-round, or triggered by specific exposures)
- What seems to make them better or worse (e.g., being outside, pet exposure, or scented products)
- Family history of allergies or asthma
- Presence of symptoms like eye itching or watery eyes
- Response to over-the-counter allergy medications
Keeping a symptom diary can be incredibly helpful. Track when symptoms appear, their severity, and any potential triggers to identify patterns over time.
Allergy Testing
If allergic rhinitis is suspected, your provider may recommend allergy testing to pinpoint specific triggers.
- Skin Prick Test: A small amount of suspected allergens is applied to your skin, usually on the forearm or back. If you’re allergic, you’ll develop a small raised bump (like a mosquito bite) at the test site.
- Blood Test (Specific IgE Test): This test measures the level of allergy-related antibodies in your blood. It’s useful for people who can’t undergo skin testing due to skin conditions or medications.
These tests help determine whether allergens are responsible for your symptoms and which ones you should avoid or treat.
When to Consider an ENT Specialist
You may need to see an ear, nose, and throat (ENT) specialist—also known as an otolaryngologist—if:
- Symptoms don’t respond to standard treatments
- You have frequent or chronic sinus infections
- You experience nasal obstruction due to structural issues (e.g., deviated septum, nasal polyps)
- You’re unsure whether your symptoms are due to allergies or something else
- Your quality of life is significantly affected by chronic congestion or sinus pressure

Treatment Options
Best Treatments for Seasonal Allergies
If you suffer from seasonal allergies, the following options can help relieve symptoms:
- Antihistamines – These medications help reduce sneezing, itching, and runny nose by blocking histamine, a chemical involved in allergic reactions.
- Nasal corticosteroids – These sprays reduce inflammation in the nasal passages, offering powerful, long-term relief when used consistently.
- Immunotherapy – Allergy shots or sublingual tablets can help desensitize your immune system over time, reducing or even eliminating allergic reactions.
How to Manage Non-Allergic Rhinitis
For non-allergic rhinitis, treatment focuses on symptom control and avoiding irritants:
- Saline rinses – Rinsing your nasal passages with saline solution can help clear out irritants and mucus.
- Ipratropium nasal spray – This prescription spray can help reduce a constantly runny nose by decreasing nasal secretions.
- Avoiding triggers – Identifying and avoiding things like smoke, strong odors, or weather changes can significantly improve symptoms.
- Lifestyle changes – Using humidifiers, HEPA air filters, and maintaining a clean living environment can minimize irritation and improve air quality.
Prevention and Lifestyle Tips
Managing Triggers Indoors and Outdoors
Controlling your environment is key to preventing allergy and rhinitis flare-ups. Here’s how to reduce exposure:
- Keep windows closed during high pollen seasons to prevent allergens from entering your home.
- Shower and change clothes after being outdoors to remove pollen or pollutants that cling to skin and fabric.
- Avoid outdoor activities in the early morning, when pollen counts are typically highest.
- Use a mask when doing yard work or cleaning dusty areas.
How to Reduce Exposure to Allergens and Irritants
- Vacuum frequently with a HEPA-filter vacuum to trap allergens like dust mites and pet dander.
- Wash bedding weekly in hot water to kill dust mites.
- Avoid strong fragrances, smoke, and chemical cleaners that can irritate your nose and lungs.
- Keep pets out of bedrooms and bathe them regularly to reduce pet dander.
Air Quality Tools and Home Hacks
- Use air purifiers with HEPA filters to clean indoor air.
- Monitor pollen and air quality levels using apps like AirVisual, Pollen.com, or your local weather service.
- Run a dehumidifier to keep indoor humidity below 50%, making your home less hospitable to mold and dust mites.
- Place allergen-proof covers on pillows and mattresses.
Final Takeaway
Know the Difference, Choose the Right Path
Seasonal allergies and non-allergic rhinitis may feel similar, but understanding their key differences is crucial for finding the right relief. Seasonal allergies are triggered by allergens like pollen and typically respond well to antihistamines, nasal sprays, and immunotherapy. Non-allergic rhinitis, on the other hand, is often caused by irritants such as smoke, scents, or weather changes and may require lifestyle changes, saline rinses, or specific nasal medications.
Don’t Guess—Get Diagnosed
If you’re unsure which condition you’re dealing with, don’t self-diagnose. A healthcare provider or allergist can perform tests to pinpoint the cause of your symptoms and help you find a personalized treatment plan.
Relief Is Possible
Living with constant sneezing, congestion, or a runny nose can feel frustrating, but it doesn’t have to be permanent. With the right diagnosis and tools, you can take control of your symptoms and feel better year-round.
Real-Life Success Stories
My journey with Non-allergic Rhinitis
This Reddit post shares the personal journey of a man who has struggled with non-allergic rhinitis (NAR) for nearly two years, starting in October 2020. The man, in his early 30s, first experienced sudden nasal congestion, which persisted even after trying various remedies like saline nasal sprays, humidifiers, and over-the-counter medications. After a few visits to doctors, including an ENT and an allergist, he was diagnosed with non-allergic rhinitis, which is characterized by congestion caused by inflamed turbinates without the presence of allergies. His congestion worsened with environmental changes, particularly humidity and temperature fluctuations, and showed slight improvement after undergoing septoplasty and turbinate reduction surgery in 2021.
Despite these interventions, the man still experiences ongoing congestion and difficulty breathing, particularly in the mornings. He has tried a wide range of medications, including corticosteroid nasal sprays (e.g., Flonase, Nasacort, Budesonide), antihistamines, nasal emollients, and even Afrin (which he uses sparingly to avoid rebound congestion). Other treatments, including capsaicin sprays and dietary changes, have shown limited or no benefits. The man suspects climate plays a key role in his symptoms, with cold, dry environments offering some relief. As a result, he plans to visit regions with drier climates to explore potential improvements in his condition.
Key Takeaways:
- Diagnosis and Symptom Timeline: Non-allergic rhinitis developed suddenly in late 2020, with persistent nasal congestion due to enlarged turbinates, but no other allergy symptoms.
- Impact of Climate: The individual noticed that colder, drier climates seem to help alleviate symptoms, leading him to consider moving or traveling to such environments for relief.
- Medical Interventions: Despite trying various treatments, including corticosteroid nasal sprays, surgery (septoplasty and turbinate reduction), and antihistamines, relief has been partial and inconsistent.
- Environmental Triggers: Humidity, temperature, and pressure changes are key triggers for worsening symptoms. Certain substances like alcohol, strong emotions, spicy foods, and hot showers exacerbate congestion.
- Ongoing Management: The individual continues to rely on a combination of medications (e.g., Singulair, Budesonide rinses, Afrin) and strategies like using the Intake Breathing Kit and staying in front of the A/C for relief.
- Next Steps: He plans to explore treatments like Omnaris, Nasonex, and Dupixent, and further investigate the relationship between diet, exercise, and his symptoms.
- Encouragement to Seek Professional Advice: The author encourages others to consult with their doctors before trying any treatments mentioned and shares his experience in the hope of helping others with similar conditions.
Chronic Allergic Rhinitis Solved
I’m a 25-year-old male, and I’ve been struggling with chronic allergic rhinitis and a deviated nasal septum for a while now. My symptoms were pretty intense—I’d sneeze at least 10-15 times a day, and if I caught a cold, it could go up to 25-30 sneezes. My nose was constantly dripping mucus, almost like a child’s, and I’d always experience post-nasal drip.
Things got worse when I ate anything even remotely spicy—the mucus in my throat would hold onto the spiciness, leaving a burning sensation in my throat.
Finally, I decided to visit an ENT doctor near my home. After an endoscopy, the doctor confirmed I had a deviated nasal septum and chronic allergic rhinitis. He told me that this condition might be with me for life, but it could be managed to reduce symptoms significantly.
The doctor prescribed some tablets and a nasal spray. When I used the nasal spray, it was like magic—my mucus production stopped, and things started returning to normal. I’ve been taking the tablets for about a week now, and it’s been a huge improvement. I can breathe easily, and my sneezing and mucus issues have pretty much disappeared. The only thing left is the deviated nasal septum, but even with that, I can now breathe well through both nostrils.
Key Takeaways:
- Chronic allergic rhinitis and a deviated nasal septum can cause persistent sneezing, mucus, and post-nasal drip.
- Spicy foods can worsen symptoms by causing burning in the throat.
- Proper treatment, including nasal sprays and tablets, can significantly reduce symptoms, improving breathing and comfort.
Dara`s Successful Recovery from Lifelong Allergic Rhinitis
Dara, a 19-year-old woman, has suffered from allergic rhinitis since she was a child, with symptoms that severely impacted her life. She couldn’t play with other kids, and her condition was further complicated by blocked sinuses, which caused pain and discomfort. She describes her childhood as a “living hell” due to these ongoing health issues.
After visiting Dr. Rinda at Maxg, Dara’s condition was thoroughly evaluated. Dr. Rinda explained the root cause of her symptoms and recommended surgery. The patient underwent a detailed procedure to clear her sinuses, correct a deviated nasal septum, and clear blockages in the frontal, maxillary, ethmoid, and sphenoid sinuses.
Following the surgery, Dara experienced significant relief. She could breathe freely for the first time in her life and expressed immense gratitude for the positive impact the surgery had on her health and well-being. She was particularly appreciative of Dr. Rinda’s solid experience and the care provided by his team.
Key Takeaways:
- Chronic Allergic Rhinitis: Long-term allergic rhinitis can severely affect a person’s quality of life, leading to difficulty breathing and limitations on daily activities.
- Sinus Blockages: Blocked sinuses can cause significant pain and discomfort, which may be exacerbated by a deviated nasal septum.
- Effective Treatment: Endoscopic surgery, including the correction of the nasal septum and clearing of sinuses, can provide significant relief and improve breathing.
- Patient Experience: The emotional and physical relief after surgery is profound, highlighting how life-changing such procedures can be for patients who have suffered from chronic sinus issues.
- Doctor-Patient Relationship: Trust in a knowledgeable and experienced healthcare professional is crucial for successful treatment outcomes.
FAQs
Can you have both seasonal allergies and non-allergic rhinitis?
Yes, it is possible to have both seasonal allergies (allergic rhinitis) and non-allergic rhinitis at the same time. In fact, some individuals may experience symptoms of allergic rhinitis during certain times of the year due to allergens like pollen, while also having ongoing symptoms of non-allergic rhinitis caused by irritants like strong odors, weather changes, or environmental factors. Managing both conditions may require a combination of treatments, including antihistamines, nasal sprays, and lifestyle adjustments.
Is non-allergic rhinitis permanent?
Non-allergic rhinitis can be a chronic condition, but it’s not always permanent. Its duration depends on the underlying cause, such as irritants in the environment, medications, or structural issues like a deviated septum. While non-allergic rhinitis may persist over time, symptoms can often be managed with lifestyle changes, nasal sprays, antihistamines, or other treatments. In some cases, surgical interventions may help alleviate long-term symptoms.
What’s the fastest way to relieve symptoms?
The fastest way to relieve non-allergic rhinitis symptoms is through the use of nasal sprays (such as saline or corticosteroid sprays), which can quickly reduce inflammation and mucus production. Over-the-counter antihistamines can help if there’s an allergic component to your symptoms. Inhaling steam or using a humidifier can also relieve congestion and dryness. For immediate relief, avoiding known triggers like smoke, strong odors, or allergens is crucial. However, for long-term symptom management, a combination of treatments and lifestyle changes may be necessary. Always consult a healthcare professional for personalized advice.
References
Mayo Clinic
Wikipedia
Cleveland Clinic
Have you ever struggled to figure out whether your symptoms are from allergies or something else?
We’d love to hear your story. Have you dealt with seasonal allergies or non-allergic rhinitis? What worked for you, and what didn’t?
Share your experience in the comments and help others find answers, too. And if this post helped you, share it with someone who needs clarity on their symptoms






Leave a Reply