Polycystic Ovary Syndrome (PCOS) is a complex hormonal disorder affecting millions of women worldwide. It can impact your metabolism, fertility, and overall health. If you’ve been diagnosed with PCOS or suspect you might have it, understanding its symptoms, treatment options, and weight management strategies is crucial for improving your quality of life.
Understanding PCOS and Its Impact on Your Health
Polycystic Ovary Syndrome (PCOS) is one of the most common hormonal disorders, affecting 1 in 10 women of reproductive age worldwide. Despite its prevalence, many women remain undiagnosed or misdiagnosed, often struggling with its physical and emotional effects without adequate support.
PCOS is not just about irregular periods or fertility challenges—it’s a metabolic and endocrine disorder that can have long-term health implications. If left untreated, PCOS can increase the risk of serious conditions such as:
- Type 2 diabetes (affecting up to 50% of women with PCOS by age 40).
- Heart disease due to high cholesterol and high blood pressure.
- Infertility caused by irregular ovulation.
- Endometrial cancer from prolonged estrogen exposure.
- Mental health disorders like anxiety and depression.
Managing PCOS requires a holistic approach—including medical treatment, dietary and lifestyle changes, and mental health support. Whether you’ve recently been diagnosed or have been struggling with symptoms for years, this guide will help you understand the condition, explore treatment options, and adopt sustainable weight management strategies for better overall health.
This precise blog post will provide you with updated and research-backed information from reputable sources like the National Institutes of Health (NIH), the World Health Organization (WHO), the Centers for Disease Control and Prevention (CDC), and scientific literature available on PubMed.
What is PCOS?
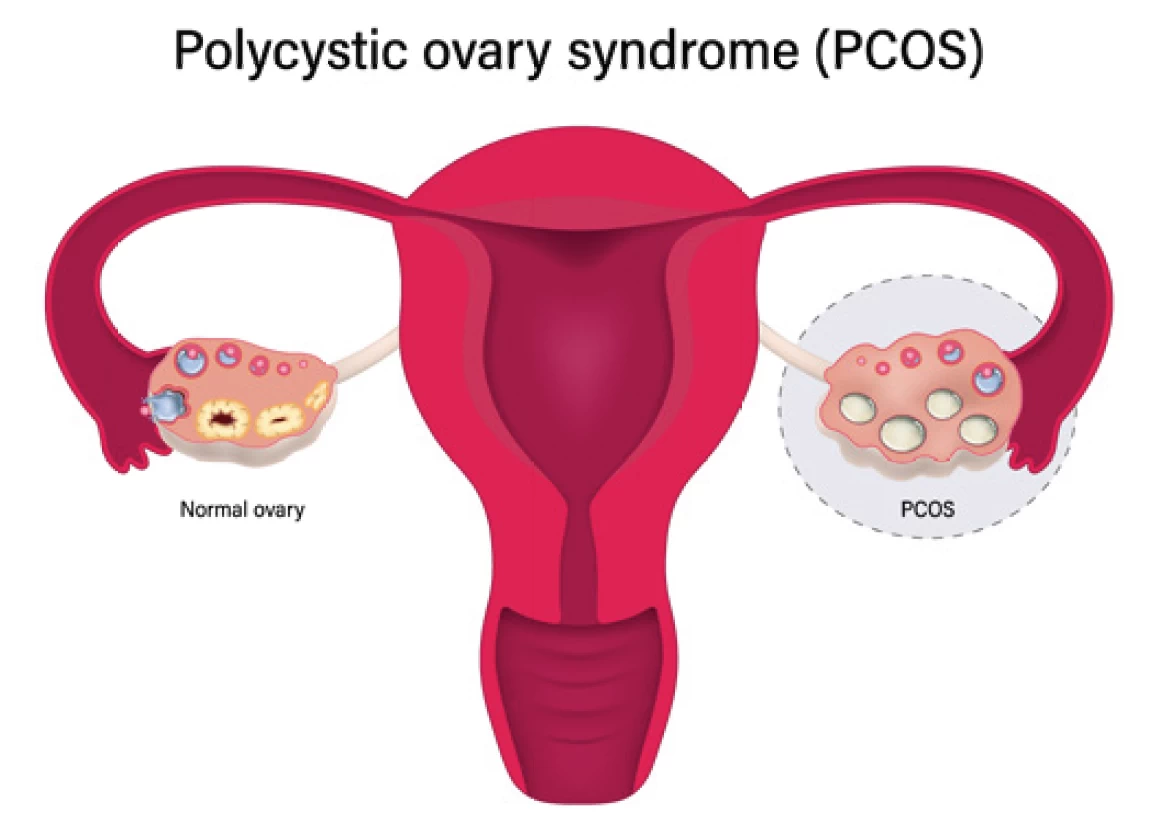
PCOS is a hormonal disorder that primarily affects women of reproductive age. It is characterized by three main features:
- Irregular or absent periods – due to disrupted ovulation.
- High levels of androgens (male hormones) – leading to symptoms like excessive hair growth (hirsutism), acne, and hair thinning.
- Polycystic ovaries – where the ovaries contain multiple small cysts and fail to release eggs regularly.
While the exact cause of PCOS remains unclear, researchers believe genetic, hormonal, and environmental factors contribute to its development.
Common Symptoms of PCOS
PCOS symptoms can vary widely from person to person. Some of the most common include:
- Irregular Menstrual Cycles: Longer or shorter cycles, skipped periods, or heavy bleeding.
- Excessive Hair Growth (Hirsutism): Unwanted hair on the face, chest, back, or arms.
- Acne and Oily Skin: Due to increased androgen levels, leading to persistent breakouts.
- Hair Thinning or Male-Pattern Baldness: Hair loss around the crown or hairline.
- Weight Gain or Difficulty Losing Weight: Often linked to insulin resistance.
- Darkened Skin Patches (Acanthosis Nigricans): Dark, velvety patches around the neck, armpits, or groin.
- Polycystic Ovaries: Enlarged ovaries with multiple follicles seen on ultrasound.
- Mood Disorders: Increased risk of depression, anxiety, and mood swings.
- Fertility Issues: Difficulty conceiving due to irregular ovulation.
Causes and Risk Factors
PCOS is linked to various factors, including:
- Genetics: If your mother or sister has PCOS, you’re more likely to develop it.
- Insulin Resistance: Many women with PCOS have insulin resistance, which increases the risk of type 2 diabetes.
- Inflammation: Chronic low-grade inflammation has been found in women with PCOS, contributing to metabolic issues.
- Hormonal Imbalances: High levels of luteinizing hormone (LH) and insulin drive excess androgen production.
Health Risks Associated with PCOS
Without proper management, PCOS can lead to long-term complications, including:
- Infertility and Pregnancy Complications – Increased risk of miscarriage, gestational diabetes, and preeclampsia.
- Type 2 Diabetes – PCOS is one of the leading causes of insulin resistance and diabetes in women.
- Heart Disease – Increased risk of high blood pressure, high cholesterol, and cardiovascular disease.
- Endometrial Cancer – Due to irregular ovulation and unopposed estrogen exposure.
- Mental Health Disorders – Higher prevalence of anxiety, depression, and eating disorders.
Source : Womenshealth.gov
Diagnosis of PCOS
There is no single test for PCOS. Diagnosis is typically made based on the Rotterdam Criteria, which require at least two of the following three conditions:
- Irregular or absent menstrual cycles.
- Elevated androgen levels (through blood tests or physical symptoms like acne and excessive hair growth).
- Polycystic ovaries seen on an ultrasound.
Your doctor may also perform additional tests to rule out other conditions, including thyroid disorders, adrenal hyperplasia, and prolactin imbalances.
Medication – Treatment Options for PCOS
PCOS treatment is individualized, depending on your symptoms and health goals. It typically includes:
Several medications can help manage PCOS symptoms:
- Birth Control Pills: Regulate menstrual cycles, reduce acne, and lower androgen levels.
- Metformin: Improves insulin resistance and helps regulate ovulation.
- Anti-Androgens (e.g., Spironolactone): Reduce excessive hair growth and acne.
- Clomiphene or Letrozole: Used to induce ovulation in women trying to conceive.
- Gonadotropins: Injectable fertility medications for severe infertility cases.
The first-line treatment for PCOS includes diet, exercise, and weight management strategies.
Source: Nichd.nih.gov
Dietary Strategies And Exercise for PCOS
Losing even 5-10% of body weight can significantly improve PCOS symptoms, restore ovulation, and enhance fertility. However, weight loss can be challenging due to insulin resistance and metabolic imbalances.
A well-balanced diet can help regulate insulin and hormone levels. Here are some evidence-based dietary recommendations:
- Low Glycemic Index (GI) Foods: Whole grains, legumes, vegetables, and lean proteins help stabilize blood sugar.
- Reduce Processed Carbs and Sugars: Minimize refined sugars, white bread, and pastries to lower insulin resistance.
- Increase Fiber Intake: Foods like leafy greens, chia seeds, and flaxseeds improve digestion and insulin sensitivity.
- Healthy Fats: Include avocados, olive oil, nuts, and fatty fish to reduce inflammation.
- Protein-Rich Foods: Chicken, fish, tofu, and eggs help balance blood sugar and keep you full longer.
- Avoid Dairy and Gluten (If Sensitive): Some women with PCOS report symptom improvement when avoiding dairy and gluten.
Regular physical activity helps manage weight and improves insulin sensitivity. Aim for:
- 150 minutes of moderate exercise per week – brisk walking, cycling, or swimming.
- Strength training – 2-3 times per week to build muscle and improve metabolism.
- High-Intensity Interval Training (HIIT) – Effective for fat loss and insulin regulation.
- Yoga and Pilates – Help reduce stress and improve hormonal balance.
Natural and Alternative Treatments
Some women find relief with complementary therapies, though more research is needed. Popular options include:
- Inositol Supplements: Myo-inositol and D-chiro-inositol improve insulin resistance and ovulation.
- Vitamin D and Magnesium: Help regulate hormone levels and improve metabolic health.
- Spearmint Tea: May reduce excessive hair growth and lower androgen levels.
- Acupuncture: Some studies suggest acupuncture may help regulate cycles and improve ovulation.
Managing PCOS-Related Stress and Mental Health
PCOS can affect your emotional well-being, making stress management essential. Consider:
- Mindfulness and Meditation – Reduce anxiety and improve mental clarity.
- Cognitive Behavioral Therapy (CBT) – Helps address negative thought patterns.
- Support Groups – Connecting with others with PCOS can be helpful.
PCOS and Fertility: What You Should Know
If you’re trying to conceive, early intervention can improve your chances. Here’s what you can do:
- Track Ovulation – Use basal body temperature (BBT) tracking, ovulation predictor kits, or fertility apps.
- Weight Management – Helps restore ovulation and increases fertility.
- Fertility Treatments – If lifestyle changes don’t work, medications like Clomid, Letrozole, or IVF may be necessary.
When to See a Doctor
Consult a healthcare provider if you experience:
- Severe irregular periods or no periods at all.
- Excessive hair growth, hair loss, or persistent acne.
- Difficulty losing weight despite lifestyle changes.
- Trouble conceiving after trying for over a year.
Source: Who.int
PCOS is a lifelong condition, but with the right management, you can improve your symptoms, fertility, and overall health. Lifestyle changes, medications, and support from healthcare providers can help you lead a healthier life.
If you suspect you have PCOS, don’t hesitate to seek medical advice. Early intervention can prevent long-term complications and improve your well-being.
Patient’s Experience
The Rioux Family’s Journey: Overcoming PCOS and Embracing Parenthood Through IVF with PGT
For many couples, the journey to parenthood isn’t always straightforward. The Rioux family bravely shared their experience with PCOS (polycystic ovary syndrome) and how in vitro fertilization (IVF) with preimplantation genetic testing (PGT) helped them achieve their dream of having a baby. Their story is one of resilience, science, and hope.
Understanding PCOS and Its Impact on Fertility
PCOS is a common hormonal disorder that affects many women worldwide. It can cause irregular menstrual cycles, ovarian cysts, and difficulties with ovulation—making natural conception challenging. For the Rioux family, this meant struggling to conceive and seeking medical interventions to grow their family.
The Role of IVF and PGT in Their Journey
After facing fertility challenges, they turned to in vitro fertilization (IVF), a process where eggs are retrieved, fertilized in a lab, and implanted into the uterus. To improve their chances of a successful pregnancy, they also used preimplantation genetic testing (PGT), which helps identify embryos free from genetic abnormalities before implantation.
The Emotional and Physical Toll of IVF
Like many couples undergoing fertility treatments, the Rioux family experienced the ups and downs of hormone treatments, injections, and the emotional weight of waiting for results. Their journey required immense patience and support, but they remained hopeful throughout the process.
Welcoming Their Baby and Life After Treatment
Through medical advancements and perseverance, they finally welcomed their baby, making all the challenges worthwhile. They emphasize the importance of after-care, including hormonal balance, postpartum recovery, and ongoing health management for PCOS. Their experience highlights the significance of support systems, lifestyle changes, and medical guidance in navigating life after IVF.
Reference Sources:
https://womenshealth.gov/a-z-topics/polycystic-ovary-syndrome
https://www.nichd.nih.gov/health/topics/pcos/conditioninfo/treatments
https://www.who.int/news-room/fact-sheets/detail/polycystic-ovary-syndrome





Leave a Reply